Resources:
Community, Genetic Reports & Natural History Study Review

TUBB4A-related leukodystrophy patients often require a range of therapies and visits to specialists to address symptoms. The extensive care demands can leave caregivers feeling drained, overwhelmed, and socially isolated. The impact of TUBB4A mutations extends beyond symptom management, affecting various aspects of family life. It's essential to build a support network, including family, friends, therapists, and respite care. Don't hesitate to seek help and share your feelings. Connect with other parents and legal guardians facing similar challenges by joining the private TUBB4A Parent Facebook group for support and understanding.
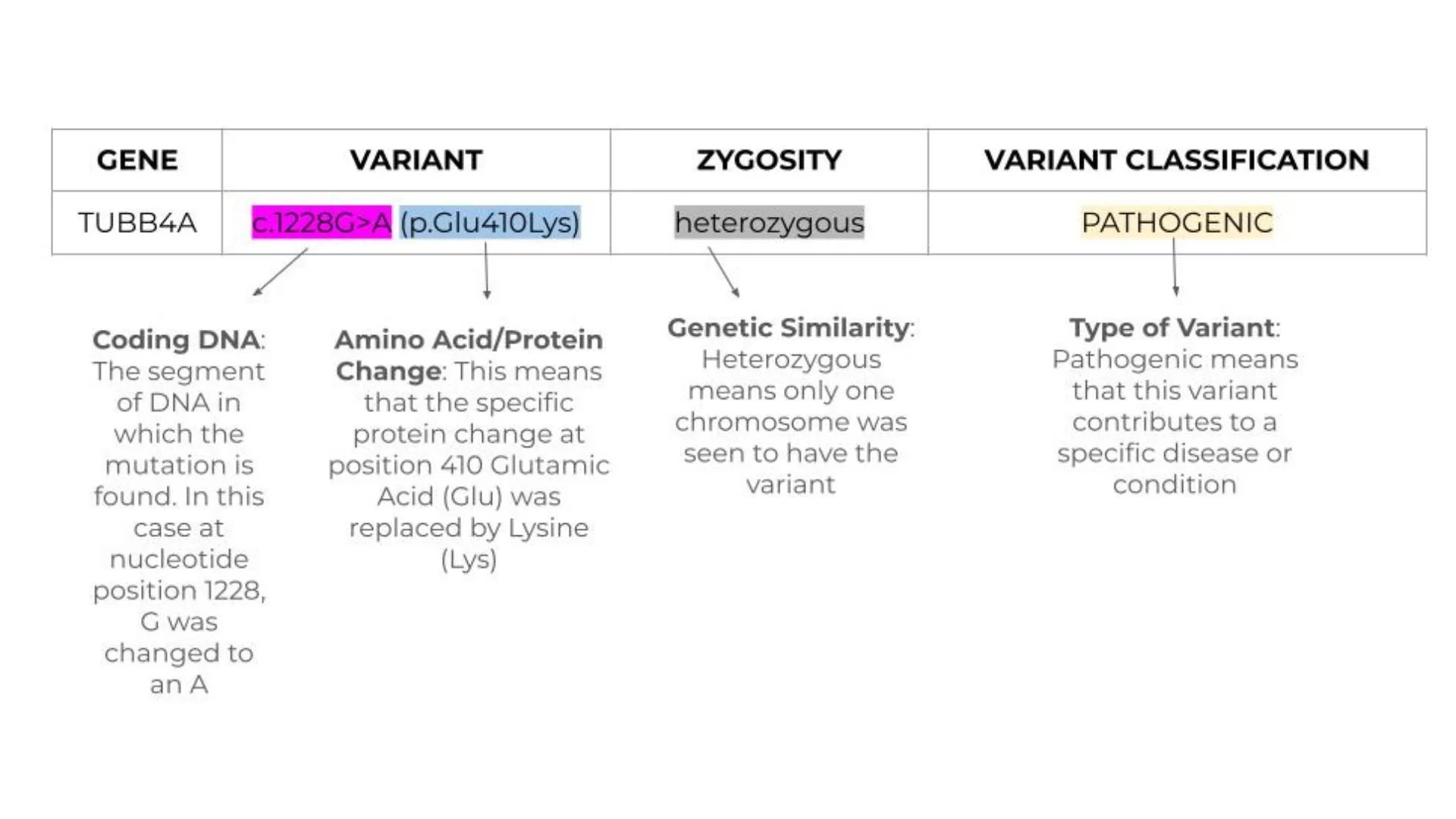
Understanding your Genetics Report
Understanding a genetic test report can feel overwhelming at first, with all the technical terms and symbols. If you're puzzled by your report, a genetic counselor is the best person to help decode it. Still, we know you might have more questions afterward, so we've put together this guide to offer further assistance.
Parent-Friendly Overview of the 2025 TUBB4A Natural-History Study
What This New Study Tells Us About TUBB4A Leukodystrophy—and Why It Matters for Your Family
A team of clinicians from five continents pulled together medical records for 216 children who have TUBB4A-related leukodystrophy, making this the largest natural-history study of our community so far. By looking at how symptoms unfolded over many years, the researchers sketched a clearer roadmap of the condition. Below is a parent-friendly digest of what they found and how you can use these insights today.
1. Three main “tracks” of the disease
The study showed that a child’s genetic change and very early motor milestones can predict how the condition progresses:
| Sub-type | How it’s identified | What the study saw |
|---|---|---|
| Early-infantile | Child cannot sit on their own by 9 months and does not carry the common p.Asp249Asn variant. | Tends to be the most severe. Only ~9% of these children ever walked independently, and complications begin earlier. |
| Late-infantile | Child can sit by 9 months and does not have p.Asp249Asn. | Most children (75%) walked; skills are lost more slowly. |
| p.Asp249Asn group | Child carries the p.Asp249Asn variant (regardless of sitting age, though most sat by 9 months). | About 80% walked, but they tended to lose skills sooner than the late-infantile group. |
2. What shows up first?
- Delayed motor milestones (e.g., rolling, sitting) were the very first sign in two-thirds of children.
- Abnormal muscle tone (stiff or floppy muscles) was next most common (43%).
- Other early clues included eye movement issues (nystagmus) and feeding difficulties.
Median age when families noticed something was wrong: about 8½ months (0.71 years).
3. Common health challenges to watch
| Issue | How often it happened | Tips for families |
|---|---|---|
| Feeding tube (G-tube) | 38 % of all children; inserted much earlier in the early-infantile group | Ask your team to screen swallowing early—even if your child is still taking bottles/food by mouth. |
| Scoliosis (curved spine) | 36 % overall; earlier in early-infantile | Regular spine X-rays and seating supports can catch curvature before it causes pain. |
| Hip dislocation | 30 % | Annual hip ultrasounds or X-rays are recommended in many clinics. |
| Seizures | 31 %; began youngest in the early-infantile group | Keep a seizure action plan and discuss rescue meds with neurology. |
| Heart findings (e.g., valve changes, aortic dilation) | about 17 % of those scanned | Consider a baseline cardiology visit even if there are no symptoms. |
4. When do skills start to fall off?
Researchers scored motor ability (GMFC-MLD scale). Severe motor decline (needing total support for head and trunk) happened at very different ages:
- ~7 years in early-infantile
- ~14 years in the p.Asp249Asn group
- ~19 years in the late-infantile group
Communication abilities followed a similar pattern, dipping sooner in the p.Asp249Asn children than in the late-infantile group.
5. What these findings mean for your child—and for research
- Better predictability. Knowing which track a child is on lets clinicians anticipate needs (feeding, orthopedic, seizure management) before problems snowball.
- Trial-ready groups. Clear sub-types help drug developers design smaller, smarter trials that compare “apples to apples.” The study authors note that subtype-based grouping will be crucial for upcoming disease-modifying therapies.
- Hope on the horizon. Because the timelines are now mapped out, researchers can pick concrete trial goals—like delaying loss of walking or reducing tube-feeding rates.
6. Take-home checklist for parents
- Track milestones early—share videos of sitting, standing, and first steps with your neurologist.
- Schedule routine swallow studies and ask when a G-tube evaluation makes sense.
- Keep eyes on the spine and hips—regular imaging can catch changes early.
- Ask for a baseline heart exam.
- Stay engaged with research. Subtype-specific studies (including ASOs and gene therapies) are in planning stages, and natural-history data like this study makes them possible.
Remember: Every child’s journey is unique. These numbers describe overall trends, not individual limits.
Have questions? The Kinslow TUBB4A Foundation is here to help. Reach out via our contact button or join the private parent Facebook page to connect with other families navigating similar paths.
This blog post is for educational purposes only and not a substitute for medical advice from your care team.
Organizations you might find helpful:
n-Lorem Foundation
~
IPSEN Cares
~
HopeKids
~
n-Lorem Foundation ~ IPSEN Cares ~ HopeKids ~